How do dentists recognize and remove decay?
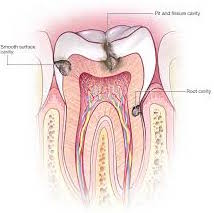
Lately I have been teaching on Thursdays and Fridays at NYU's school of dentistry. The students often ask for tips on how to recognize decay and how to tell when a tooth it is completely removed. The answer is not simple and not all dentists employ the same exact criteria. Decay is a process that affects dentin, in which both dentin is demineralized and invaded by bacteria. Decay can appear to be different colors depending on what it is stained by. Decay that has been present for a long while, say six months- years, usually has a orange or brownish appearance, some some decay can actually have a similar color to naturally occurring dentin. Often it is not fully visible when a dentist performs their clinical exam and it can be covered by healthy looking enamel. Even when it is visible on a tooth's surface, often the decay visible is on the tip of a proverbial iceberg, and the amount of actual decay is much larger. When viewed on a radiograph interproximal decay can be seen as a darkening on the tooth since demineralized tooth looks darker on a radiograph than healthy dentin.
Most of the time, to better visualize the decay, an opening is made in the tooth enamel using a carbide bur and a high speed drill. Once a large enough initial opening is made the decay can be excavated using a sharp dental instrument called a spoon excavator or a low speed carbide round bur. Since the decay is softer than healthy dentin, these tools will more or less selectively remove the decayed portion. If the decay is extensive a wider open may have to be established since there is often decay still difficult to access, hiding under intact enamel. Once a "healthy margin" can be established along the walls of the preparation, then any residual decay can be fully removed using the spoon excavator or low speed round bur.
Some dentists employ a red dye called "caries detector" that will stain demineralized internal tooth structure to more easily determine when a tooth is cleaned of decay. In my opinion, this is a great adjunct tool, but should be used with good clinical judgement, especially in deeper caries excavations, so that pulpal exposures are minimalized. Often when cleaning out extremely deep cavities some slightly soft "affected dentin" is purposely left behind, if it is immediately adjacent to the tooth's pulp. I place a layer of dycal and another layer of glass ionomer liner over it before placing a filling. The affected dentin I leave is usually is not extremely soft, but instead is relatively hard ( but if it wasn't immediately next to the pulp I would normally remove it ).
Dentists don't examine this layer with a microscope, so there is no real way of telling whether this tooth is "sterile" or if it has some bacteria present, so covering it with a couple of layers of medicamentl seems prudent, since these tend to desiccate and seal the affected area . This type of treatment affected dentin is sometimes termed an indirect pulp cap (as opposed to a direct pulp cap where the pulp is actually exposed during the removal of decay).
from Ask Dr. Spindel - http://lspindelnycdds.blogspot.com/2019/02/how-do-dentists-recognize-and-remove.html - http://lspindelnycdds.blogspot.com/
Comments
Post a Comment