Dental & Oral Surgery: Exposing Everything for a Fear-Free Visit
Hearing that you need dental surgery can feel overwhelming at first.
With all the types and treatments available for oral & maxillofacial surgery, it’s normal to have questions. You’re likely wondering about average costs, available options, preparation, and how to shorten your recovery time.
In this article, we’ll tackle all 12 types of dental surgery, the reasons and costs behind them, and the best ways to set yourself up for success both before and after surgery.
I’ll even guide you through the common questions I hear as a dentist and how to choose the best surgeon. Take a deep breath — you’re about go from overwhelmed to informed.
Reasons for Oral/Dental Surgery
The reasons for oral surgery are as numerous and individual as the patients getting them.
For some, it’s needed to repair damage caused by gum disease or tooth decay. In other cases, facial trauma or wisdom teeth may have impacted their oral health in unexpected ways. We’ll discuss the reasons for each surgery below.
12 Types of Dental Surgery
There are many different types of dental surgery, but the classifications for them can vary. Many times, the categories for oral and dental surgery are determined by the person writing that particular list. This ambiguity can get confusing, so I’m keeping it simple.
Here, I’ll walk you through all of the 12 types of oral surgery, their cost, reasons, and recovery times. The primer will help you make informed decisions when considering your options.
Before reading, please note that these costs are national averages without insurance, but your specific price will be determined by your location, needs, and individual dentist.
Here is a dental surgery list that contains everything you need to know about the types of dental surgery.
1. Endodontic Surgery
Cost:
- $80-$300 for a pulpotomy/pulpectomy
- $900-$1,300 for an apicoectomy
- $2,000-$3,000 for a root canal and crown
Reasons for Surgery: A pulpotomy/pulpectomy may be available for patients whose pulp is salvageable, but has become infected in a small area (pulpitis). In more serious cases, a root canal could be needed to treat a tooth whose roots have become infected by a wide-spreading cavity.
Finally, an apicoectomy may be needed if a root canal treatment has failed and the root tip has become reinfected.
Average Recovery Time: Pain for a few days, which should decrease along with inflammation. It may be wise to take a day off work and rest the mouth.
Endodontic surgeries are required for cases of decay or infection where the issue has penetrated the enamel. These are more serious problems that require more than a filling to treat, and cannot be reversed through remineralization.
Most of these procedures are fairly simple and common in the world of dental care. The AEA’s most recent estimates conclude that 22.3 million endodontic surgeries are performed each year.
2. Prosthodontics
There are four major types of prosthodontics: dental implants, dentures, bridges, and implant-supported prostheses.
Dental Implants
Cost: $3,000-$5,000 per tooth
If a jawbone graft is needed to stabilize the extraction site before an implant (a form of dentoalveolar surgery), it can add between $200-$1,000 to the cost.
Reasons for Surgery: Prosthodontics are needed to preserve the jawbone, prevent any shifting or malocclusion, and to provide a permanent solution with great success rates after tooth loss.
Average Recovery Time: 5-7 days for swelling to go down, though normal activities can typically be resumed after two days.
Note: a dental implant generally requires several visits. You’ll have to wait a while after the tooth extraction for the implant, and the permanent crown will need to wait before placement as well.
If saving the natural teeth isn’t an option, this is almost always where I steer my patients. Implants are typically the best of your tooth replacement options after most tooth extractions.
Not only do they have a 96% success rate, but they are usually a lifelong solution that prevents many problems that come with missing teeth.
Dentures
Cost:
- A full set of dentures can range between $1,000-$4,000
- Premium dentures average $8,000
- Partial dentures range from $500 to $1,500
You will also need to pay for extractions, which can average $75-$450 per tooth.
Reasons for Surgery: Your natural teeth are no longer feasible to use, and you need a full set of new false teeth.
Average Recovery Time: The extractions will need between 7-10 days to heal, and it will take a few weeks to get used to the feeling of dentures.
While dentures aren’t my first choice for patients, if a great deal of extractions are needed, dentures may be an affordable option. Full and partial dentures are available, based on the number of missing teeth, and can restore self-esteem and the ability to smile, chew, and speak properly.
Bridges
Cost: $2,000-$5,000
Reasons for Surgery: To cover the hole a missing tooth leaves and to prevent bite problems or shifting after extraction.
Average Recovery Time: This requires multiple visits. Recovery from soreness and swelling may take 5-7 days for the extraction, 1-2 days for the crown placement, and 1-2 days for the bridge placement.
There are four types of bridges available: traditional, Maryland, cantilever, and implant-supported, which are discussed in depth in this article. The cost is lower than an implant, making it a viable option for those who need a less-expensive prosthesis.
The option of a bridge can provide long-lasting support and prevent shifting from empty extraction sites. This is only an option if most of the surrounding teeth are still intact.
Implant-Supported Prosthesis
Cost: The number of implants needed is a critical factor in pricing.
- Implant-supported bridges can cost around $5,000-$15,000
- Implant-supported dentures run around $10,000-$15,000, depending on the material used to make the replacement teeth
Reasons for Surgery: A more permanent solution to the problems that cause the need for bridges and dentures.
Average Recovery Time: Similar to that of an implant, but with an additional 2-3 days for recovery from denture or bridge placement — 7-10 days.
Implant-supported prostheses are a more sturdy and lasting solution, though most costly. These use dental implants to anchor down the bridge or denture. This option is pricier, but I recommend it if possible.
3. Surgical Extraction/Wisdom Teeth
Cost: $75-$200 for each typical tooth; $225 to $600 for each impacted tooth
Reasons for Surgery: Shifting, improper eruption, or decay in the wisdom teeth (sometimes called third molars). Tooth extraction reasons can include a tooth that is broken, decayed, or damaged beyond repair.
Average Recovery Time: For wisdom teeth removal, 3-5 days when no impaction or dry socket occurs. For a tooth extraction, 2-3 days. However, the extraction site will take much longer to heal.
I recommend orthotropics for your child, a field of orthodontics that directly covers the growth of the palate and often prevents the need for braces and wisdom tooth removal. However, this isn’t always possible, and sometimes extractions are needed.
I also typically don’t recommend an extraction unless the natural tooth is absolutely beyond salvaging. My recommended next surgical step after extractions (other than a wisdom tooth) is an implant.
4. Periodontal Surgery
Cost:
- Gum tissue grafts are $600-$1,200 for a single tooth
- Pinhole surgery can cost between $4,000-$10,000, depending on the level of damage
- Flap surgery or pocket reduction costs between $1,000-$3,000
As with tooth implants, bone grafting may be needed if the gum disease has damaged the surrounding tooth or jawbone. This can cost another $200-$1,000.
Reasons for Surgery: Deep tartar, receding gum tissue, or problematic pockets in the gums due to periodontal disease.
Average Recovery Time: 7-10 days for flap surgery and gum tissue graft, up to 6 weeks for pinhole surgery.
Periodontal surgery aims to treat gum disease, saving you from problems like pockets of infection, receding gums, or weakening bone around the tooth’s roots. You can prevent periodontal disease through proper checkups and taking good care of your dental health.
Most of these procedures involve going beneath the gum line, which will also require stitches and delicate aftercare. Periodontics make it possible to save your teeth and gums from tooth loss and further infection.
5. Orthognathic Surgery
Cost: Between $20,000-$40,000, depending on if one or both jaws need operation and the complexity of the procedure
Reasons for Surgery: When the position of the jaw and teeth causes issues with eating, breathing, speaking, pain, or sleep.
Average Recovery Time: 3 weeks
Jaw misalignment can cause a myriad of issues, from intense facial pain to difficulty chewing, sleeping, and talking. Orthognathic surgery, or corrective jaw surgery, can move the upper and lower jaw into correct alignment and is usually used in conjunction with orthodontics.
In most cases, this maxillofacial surgery can be performed from the inside of the mouth to avoid large scars. The surgeon will move the jawbone into position and secure it, then close the incision.
6. TMJ Surgery
Cost:
- $300-$1,000 for arthrocentesis to clean out the joint
- $5,000-$7,000 to repair the damaged temporomandibular joint with arthroscopy
- A modified condylotomy could cost between $15,000-$30,000
- Open joint surgery could be $5,000-$15,000
Reasons for Surgery: Difficulty chewing or speaking, lockjaw, or extreme pain.
Average Recovery Time: For arthroscopy or arthrocentesis, you may want to wait 1-2 days to return to work, or more if your job requires a lot of speaking. Open joint surgery or a modified condylotomy will need about a week of recovery time.
The pain and inflammation that come with a severe case of TMJ are nothing to be envied. While there are physical therapies, lifestyle changes, and injections available for TMJ disorders, surgery is an option for severe cases.
Arthrocentesis and arthroscopy are less invasive options to clean or repair the damaged joint. However, if those aren’t successful, a modified condylotomy or open joint surgery may provide relief by repositioning or increasing the range of motion in the joint.
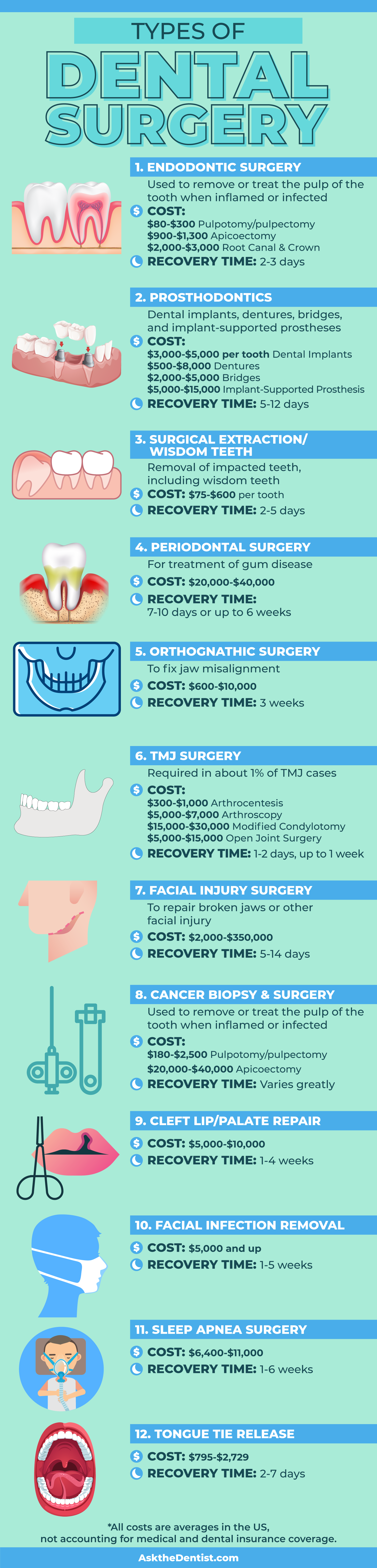
7. Facial Injury Surgery
Cost:
- As little as $2,000 for a broken jaw
- Up to $350,000 for a facial reconstruction
As you can see, the price varies dramatically, based on the injury.
Reasons for Surgery: Facial injuries that will not heal on their own or put the patient at immediate risk due to severe pain, swelling, numbness, bleeding, and difficulty chewing or talking.
Average Recovery Time: 5-7 to decrease swelling, and 10-14 days for bruising to fade. Several months of recovery time may be needed to fully heal.
The term facial trauma can include a broken upper or lower jaw, several teeth that have been knocked out, damage to the palate, and more. These traumatic injuries are typically considered medical emergencies and should be treated immediately.
Depending on the degree of reconstruction needed, the pricing for treating facial injuries can vary drastically.
8. Head/Neck/Oral Cancer Biopsy & Surgery
Cost:
- A biopsy for head, neck, or oral cancer can cost between $180-$2500, depending on the type needed
- Needle or brush biopsies, when possible, cost less than surgical extraction biopsies
- Surgery for throat cancer runs typically between $25,000-$40,000, and oral cancer typically $20,000-$30,000. However, the stage of the cancer and location will determine price.
Reasons for Surgery: A biopsy can test a concerning mass for cancer, and surgical removal of cancerous lesions can improve treatment outlook.
Average Recovery Time: This varies widely depending on the type, stage, and location of the cancer. A biopsy will typically take up to a week to recover from while you care for the wound. The pain should begin to subside after 2-3 days.
The time, cost, and measures needed to treat this condition are dependent on the location, type, and stage of cancer. For stage 1 and 2, surgery to remove the lesion and radiation treatment will likely be needed.
In later stages, parts of the jawbone, tongue, or lymph nodes may need to be removed as well. It’s important to be informed and aware about head, neck, and oral cancer to prevent the spread of this disease.
9. Cleft Lip/Palate Repair
Cost: Cleft lip or palate repair ranges from $5,000-$10,000 per surgery. If both a cleft lip and palate exist, treatment will generally require two surgeries.
Reasons for Surgery: A lip, palate, or both that did not form properly in the womb.
Average Recovery Time: 1-2 weeks for swelling to improve and roughly four weeks for the incision to heal.
Cleft lip or palate occurs when the sides of the palate, lip, or both do not fuse together during early fetal development. This can cause hearing loss, eating problems, speech issues, and dental difficulties.
This surgery can be done around three months of age for cleft lip, and nine months to one year for cleft palate. The surgeon will make incisions on either side of the cleft, pull tissue down, and close the opening. Early intervention is key, and orthodontic care will likely be necessary as well.
10. Facial Infection Removal
Cost: $5,000 and upwards, depending on the severity of the infection.
Reasons for Surgery: Certain infections of soft tissues that may be fatal if left untreated.
Average Recovery Time: 1-5 weeks, depending on the severity of infection.
Facial infections can occur from a number of causes: fungal overgrowth, bacterial infection, or even a serious dental abscess from an untreated tooth that has made its way to the face. Any facial infection should be treated right away to avoid life-threatening complications.
11. Sleep Apnea Surgery
Cost: $6,400-$11,000
Reasons for Surgery: Sleep apnea consequences like stopped breathing during sleep, collapsed airway, and poor sleep quality or cardiovascular problems resulting from the condition.
Average Recovery Time: 1-2 weeks to resume normal activities, and 3-6 weeks to fully recover.
This is one of the more involved surgeries on the list. Sleep apnea surgery involves treating the individual’s sleep apnea causes including tongue, nose, uvula, palate, and even neck or jawbone problems.
Each case is different, and a consultation can help diagnose what areas of treatment will bring you relief. This surgery will warrant a few days in the hospital and a few weeks of recovery time.
12. Tongue Tie Release
Cost: $795-2729 for a frenectomy (severing the tie in infants) or more for a frenuloplasty (a more involved procedure to severe a thick tongue tie)
Reasons for Surgery: The band of tissue under the tongue (also called a tongue tie) restricts its movement and ability to rest properly.
Average Recovery Time: 2-7 days for wound healing.
Releasing a tongue tie can relieve chronic jaw pain, facial pain, headaches, bruxism, and more. Long-term, those with a tongue tie are more likely to develop sleep apnea and airway issues.
A tongue tie release is a fairly simple surgical procedure. A laser or scalpel is typically used to sever the tie, and myofunctional therapy before and after surgery will be used to strengthen the mouth and tongue. Learn more here.
Choosing a Surgeon
Choosing a surgeon can be a tricky decision, as your smile is in their hands. Here are some considerations I recommend looking for when deciding on your oral surgeon:
- Cut down on costs by choosing a surgeon covered by your medical insurance, if you have it. Even within your network, it’s not a bad idea to cost-compare.
- For more in-depth surgeries, be sure your surgeon is certified by the American Board of Oral and Maxillofacial Surgery. This ensures you’re seeing a qualified specialist who has certified at a high level of continuing knowledge and education.
- Talk with your dentist. They’ve likely worked with many oral and maxillofacial surgeons over the years, and can provide an educated referral.
- When you visit the oral surgeon for a consultation, see what they recommend — is it lining up with your dentist’s recommendations? Do you feel comfortable asking questions? This is your mouth, after all.
- Look for a specialist in their field. We’ll cover the available specialties below.
Wondering about choosing a dentist, too? Here’s my list of what to look for.
Prepping for Dental Surgery
I always say that your oral health is a depiction of your overall health. Preparing for dental surgery starts from the inside out. You may be surprised to hear me say that your diet is actually one of the most powerful tools you have to optimize your surgery preparation and recovery.
All the changes in your mouth will likely produce inflammation, but here’s the good news: plant-based foods, essential fatty acids, and high-antioxidant foods all support reduced inflammation. This is not only true for your mouth, but the whole body.
When the body is less busy fighting inflammation, it can focus on what’s important: healing.
Adopting an anti-inflammatory diet of whole grains, fruit, and vegetables, getting your fatty acids like omega-3s in salmon and pastured eggs, and adding in some turmeric will reduce inflammation after surgery naturally.
Your dental hygiene before the surgery is another way you can help your mouth prepare. I encourage you to brush your teeth properly and floss like your mouth depends on it — because it does. The better your oral hygiene now, the better your mouth will fare after surgery.
You can prevent complications and reduce your inflammation before you even go in for surgery using these tips. You’ll be glad you tried an anti-inflammatory diet and better oral hygiene when your mouth is bouncing back beautifully.

Anesthesia: Types & Preparation
With oral surgery, you have a host of options for anesthesia:
- Local anesthesia: For smaller procedures like crown fittings, bridge placements, or endodontics, local anesthesia may suffice. This option can provide shorter recovery time in outpatient procedures, and is becoming more sophisticated each year.
- IV sedation: Your consciousness will be suppressed and your memory of the procedure will be hazy. This is used in conjunction with local anesthesia, often in cases of multiple extractions. The sedation will take several days to fully leave the body.
- General anesthesia: This is necessary for more major surgeries, and you will feel no pain or memory of the procedure. This is recommended for major dental surgery, such as orthognathic surgery.
- Nitrous and local: You may not need sedation or anesthesia, but feel nervous about the procedure. You may be able to request nitrous oxide, which has a lower cost than sedation and wears off almost immediately.
The amount and type of anesthesia is a discussion you should have with your surgeon before treatment. If you are nervous, they may be able to recommend the type of anesthesia best for you, though in some more severe surgeries your options will be limited to general anesthesia.
Thankfully, the administration and options for anesthesia become more sophisticated each year. The amount of anesthesia needed can be determined by several things: the size of the patient, the state of their oral hygiene, any special needs, and even being a redhead.
Since sedation and anesthesia (or plain dental anxiety) can upset the stomach and nerves, I recommend CBD.
Dental Surgery Recovery
Coming prepared to dental surgery sets you up for a successful recovery. Here are my top tips for before, during, and after your procedure.
Remember, the seriousness of dental surgery varies greatly, so be realistic with your recovery timeframe and plans based on the procedure you need.
What to Do the Day of Your Surgery
The day of your surgery, make sure you have a ride to and from the procedure if you are planning to undergo sedation or general anesthesia. Also, eat something if you’re undergoing local anesthesia, but avoid food and all liquids if you are being sedated or undergoing general anesthesia.
Ask your surgeon if you should take your normal medications within the 24 hours before the surgery. They will be aware of any potential drug interactions.
Make sure you have surgeon-approved foods stocked up at home, and dress comfortably.
Finally, go in with a clean mouth, as you likely won’t be able to brush, floss, or tongue scrape for at least a few days after surgery.
What to Expect After Dental/Oral Surgery
If you’ve been sedated or under general anesthesia, you’ll likely need some time to recover before heading home. You may even need to stay at the hospital overnight if you’ve had major surgery.
You’ll want to go easy on your mouth: avoid spitting, swishing, sucking, and smoking. You’ll want to know ahead of time what oral hygiene is allowed as well to avoid damaging the surgery site.
While your surgeon will likely prescribe you some opioids, I recommend weaning off of those as quickly as possible. It’s possible to become addicted within five days, and dental surgery is a common source.
This is yet another reason I recommend CBD for natural pain management.
Remedies for Fast Recovery
- Stay hydrated! Lukewarm water helps the body recover and prevents cavities while brushing and flossing are limited. You may also try coconut water, which is rich in electrolytes and other important nutrients.
- Limit activity. Straining can cause bleeding and dislodge blood clots in the mouth. Trust me, you don’t want dry socket.
- Avoid solid foods. Your surgeon will tell you when it’s safe to chew again. Stick to the treatment plan to optimize healing.
- Stay aware. If you notice fever, pus, bleeding, or new swelling, call your surgeon. Ignoring these symptoms will certainly not speed up recovery.
Oral Surgeon Specialties
There are several specialties within oral surgery, each of which takes additional education.
All oral surgeons are trained to treat the surgeries for jaws, head, neck, and place implants. However, some oral surgeons pursue two year fellowships in these relevant specialties:
- Head and neck cancer — can include biopsies, removal of the mass, and reconstruction.
- Craniofacial surgery and pediatric maxillofacial surgery — can address cleft lip and palate.
- Cranio-maxillofacial trauma — addresses traumatic injuries to the soft tissues or skeleton.
Training for an oral surgeon includes 2-4 years of undergraduate study, four years of dental school, and four years of residency.
Finally, two more years will be necessary for a medical degree. Cosmetic specialties are also available, but not relevant to this subject.
Emergency Dental Surgery
Sometimes, emergency dental surgery can be required.These cases can include:
- Teeth that are knocked out
- Accidents/falls/blows that fracture the jaw
- A jaw dislocation
- Serious cuts and bleeding inside or around the mouth
- An abscess or infection that is swelling or causing fever or trouble breathing
If any of these happen to you, head to the ER immediately.
FAQs
Will I need to take antibiotics to prepare for dental surgery?
Is a dental surgeon the same as an oral surgeon?
Is oral surgery painful?
More involved procedures like jaw surgery or facial reconstruction may be slightly painful as you recover, but proper aftercare will keep pain under control.
Key Takeaways: Dental Surgery
The 12 types of dental surgery may be needed in different situations, but a great oral surgeon can assist in treating everything from mouth cancer to wisdom teeth. Take your time and consider your insurance, diagnosis, and dentist’s recommendation when choosing a dental surgeon.
Preventive care through diet and good hygiene and an educated anesthesia choice can alleviate nerves before the big day.
Aftercare should include limited activity, hydration, and a soft or liquid diet. Choosing a specialist and being aware of what constitutes a dental emergency are also important considerations.
Read Next: Oral Cancer: Diagnosis, Stages, Treatments, Prevention & More18 References
- Charyeva, O., Altynbekov, K., Zhartybaev, R., & Sabdanaliev, A. (2012). Long-term dental implant success and survival–a clinical study after an observation period up to 6 years. Swedish dental journal, 36(1), 1-6. Abstract: https://www.ncbi.nlm.nih.gov/pubmed/22611899
- Monje-Gil, F., Nitzan, D., & González-Garcia, R. (2012). Temporomandibular joint arthrocentesis. Review of the literature. Medicina oral, patologia oral y cirugia bucal, 17(4), e575. Full text: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3476018/
- Werther, J. R. (2004). Modified condylotomy. Journal of Oral and Maxillofacial Surgery, 62, 100. Abstract: https://www.joms.org/article/S0278-2391(04)00577-4/fulltext
- Siemionow, M., Gatherwright, J., Djohan, R., & Papay, F. (2011). Cost analysis of conventional facial reconstruction procedures followed by face transplantation. American Journal of Transplantation, 11(2), 379-385. Abstract: https://www.ncbi.nlm.nih.gov/pubmed/21272241
- Davis, G. E., Schwartz, S. R., Veenstra, D. L., & Yueh, B. (2005). Cost comparison of surgery vs organ preservation for laryngeal cancer. Archives of Otolaryngology–Head & Neck Surgery, 131(1), 21-26. Abstract: https://www.ncbi.nlm.nih.gov/pubmed/15655180
- Amponsah, E. K., & Donkor, P. (2007). Life-threatening oro-facial infections. Ghana medical journal, 41(1), 33. Full text: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1890536/
- O’Shea, J. E., Foster, J. P., O’Donnell, C. P., Breathnach, D., Jacobs, S. E., Todd, D. A., & Davis, P. G. (2017). Frenotomy for tongue‐tie in newborn infants. Cochrane Database of Systematic Reviews, (3). https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6464654/
- Galland, L. (2010). Diet and inflammation. Nutrition in Clinical Practice, 25(6), 634-640. Abstract: https://www.ncbi.nlm.nih.gov/pubmed/21139128
- Calder, P. C. (2017). Omega-3 fatty acids and inflammatory processes: from molecules to man. Biochemical Society Transactions, 45(5), 1105-1115. Abstract: https://www.ncbi.nlm.nih.gov/pubmed/28900017
- Arulselvan, P., Fard, M. T., Tan, W. S., Gothai, S., Fakurazi, S., Norhaizan, M. E., & Kumar, S. S. (2016). Role of antioxidants and natural products in inflammation. Oxidative medicine and cellular longevity, 2016. Full text: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5075620/
- Watzl, B. (2008). Anti-inflammatory effects of plant-based foods and of their constituents. International journal for vitamin and nutrition research, 78(6), 293-298. Abstract: https://www.ncbi.nlm.nih.gov/pubmed/19685439
- Agarwal, K. A., Tripathi, C. D., Agarwal, B. B., & Saluja, S. (2011). Efficacy of turmeric (curcumin) in pain and postoperative fatigue after laparoscopic cholecystectomy: a double-blind, randomized placebo-controlled study. Surgical endoscopy, 25(12), 3805-3810. Abstract: https://www.ncbi.nlm.nih.gov/pubmed/21671126
- Hawkins, J. M., & Moore, P. A. (2002). Local anesthesia: advances in agents and techniques. Dental clinics of North America, 46(4), 719-32. Abstract: https://www.ncbi.nlm.nih.gov/pubmed/12436827
- Casati, A., & Putzu, M. (2005). Anesthesia in the obese patient: pharmacokinetic considerations. Journal of clinical anesthesia, 17(2), 134-145. Abstract: https://www.ncbi.nlm.nih.gov/pubmed/15809132
- AYasny, J. S. (2009). Perioperative dental considerations for the anesthesiologist. Anesthesia & Analgesia, 108(5), 1564-1573. Abstract: https://www.ncbi.nlm.nih.gov/pubmed/19372337
- Dougherty, N. (2009). The dental patient with special needs: a review of indications for treatment under general anesthesia. Special Care in Dentistry, 29(1), 17-20. Abstract: https://www.ncbi.nlm.nih.gov/pubmed/19152563
- Liem, E. B., Lin, C. M., Suleman, M. I., Doufas, A. G., Gregg, R. G., Veauthier, J. M., … & Sessler, D. I. (2004). Anesthetic requirement is increased in redheads. Anesthesiology, 101(2), 279. Full text: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1362956/
- Phillips, J. K., Ford, M. A., Bonnie, R. J., & National Academies of Sciences, Engineering, and Medicine. (2017). Trends in Opioid Use, Harms, and Treatment. In Pain Management and the Opioid Epidemic: Balancing Societal and Individual Benefits and Risks of Prescription Opioid Use. National Academies Press (US). Full text: https://www.ncbi.nlm.nih.gov/books/NBK458661/
The post Dental & Oral Surgery: Exposing Everything for a Fear-Free Visit appeared first on Ask the Dentist.
from Ask the Dentist https://askthedentist.com/dental-surgery/

Comments
Post a Comment